Universal Basic Healthcare: A New American System
Meeting Essential Health Needs While Preserving Choice and Innovation
Howard Roark
12/31/202514 min read
Healthcare in America stands at a crossroads. We spend more per capita than any nation on Earth, yet millions struggle to access basic care. Emergency rooms overflow with patients seeking routine treatment. Families face bankruptcy over medical bills. Chronic conditions go unmanaged until they become crises. Meanwhile, our population grows sicker, with rates of obesity, diabetes, and metabolic disease reaching epidemic proportions.
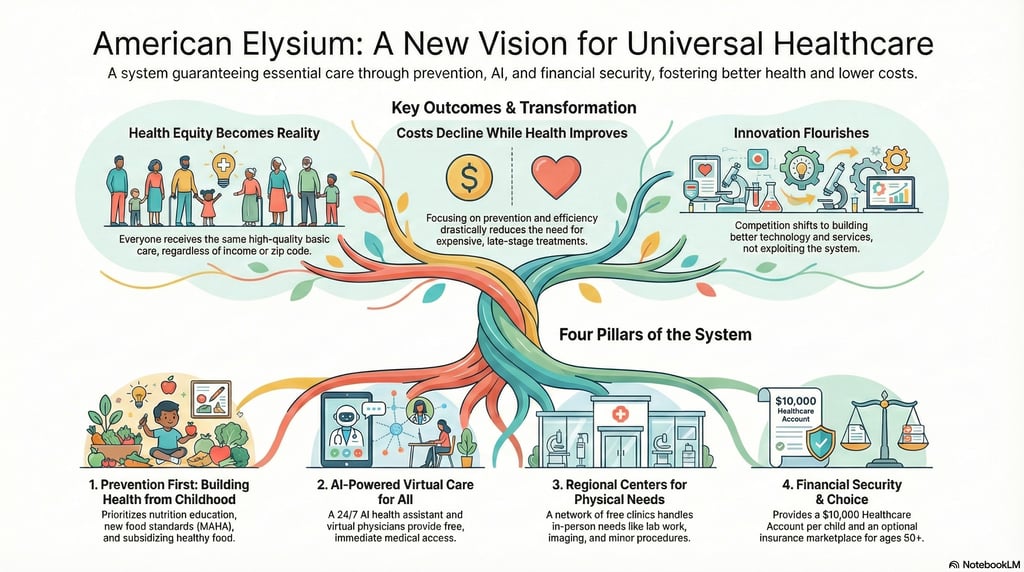
American Elysium proposes a different path: Universal Basic Healthcare that guarantees every American access to essential medical services while addressing the root causes of disease through nutrition, education, and prevention. This is not government-run healthcare or a single-payer system. It is a comprehensive approach that recognizes simple truths: in the 21st century, basic healthcare should be as accessible as clean water, preventing disease is better than treating it, and modern technology makes both possible.
Prevention First: Building Health from Childhood
The foundation of any successful healthcare system is a healthy population. Universal Basic Healthcare begins not in hospitals or clinics but in schools and communities, building health literacy and healthy habits from the earliest ages.
Comprehensive Physical and Wellness Education
Every American child will receive comprehensive physical and wellness education starting in elementary school and continuing through high school. This is not traditional PE class with dodgeball and laps. This is systematic education in how the human body works, how nutrition affects health, how exercise builds strength and resilience, and how to maintain physical and mental wellness throughout life.
Students learn practical skills: how to read nutrition labels, how to prepare healthy meals, how to recognize and manage stress, how to establish exercise routines they can maintain as adults, basic anatomy and physiology so they understand their own bodies, and the connection between lifestyle choices and long-term health outcomes.
Physical education becomes genuine education in physicality, teaching students multiple forms of movement from strength training to yoga, from team sports to individual fitness, ensuring every student finds physical activities they enjoy and can continue throughout life. The goal is not producing athletes but producing adults who understand that physical activity is as essential as sleep and nutrition.
MAHA: Make America Healthy Again
At the heart of disease prevention is nutrition, and at the heart of nutrition is food quality. Universal Basic Healthcare embraces and implements the principles of Make America Healthy Again (MAHA), establishing new standards for what Americans eat and how food is produced.
MAHA guidelines establish clear, science-based nutrition standards that prioritize whole foods over processed products, eliminate harmful additives and chemicals that have been banned in other developed nations but remain legal in American food, reduce added sugars in manufactured foods, increase transparency in food labeling, and promote regenerative agriculture practices that produce more nutritious food while improving soil health.
These are not recommendations. They are standards that food manufacturers must meet. The era of allowing companies to profit from making Americans sick is over. Food should nourish, not harm, and our regulatory framework will finally reflect that principle.
Subsidizing Health, Discouraging Disease
Universal Basic Healthcare aligns economic incentives with health outcomes. High-quality, nutritious food becomes more affordable through subsidies, making the healthy choice the easy choice for all Americans regardless of income.
Fresh fruits and vegetables, high-quality proteins, whole grains, and other nutrient-dense whole foods receive subsidies that reduce their cost at retail. Farmers markets accept benefits programs. Community-supported agriculture (CSA) programs become accessible to all income levels. The goal is simple: healthy food should cost less than junk food, not more.
Simultaneously, foods that actively harm health face financial disincentives. Products high in added sugars, processed foods loaded with chemicals and preservatives, and items that fail to meet nutritional standards face additional taxes that reflect their true cost to public health. This is not punishment but honest accounting. When a product contributes to obesity, diabetes, and heart disease, the price should reflect the healthcare costs society eventually bears.
The food industry will adapt, as it always does. Companies will reformulate products to meet new standards. New businesses will emerge to provide healthy alternatives. Innovation will flow toward making nutritious food convenient and delicious rather than making junk food cheaper and more addictive. Market forces, properly aligned, will work for health rather than against it.
The Foundation: AI-Enhanced Virtual Care
The cornerstone of Universal Basic Healthcare is revolutionary but simple: every American can connect with medical care anytime, anywhere, at no cost. This care combines cutting-edge artificial intelligence with human medical expertise to deliver a level of service impossible in traditional healthcare.
Your AI Health Assistant
Every American receives access to an advanced AI health assistant, available 24/7 through smartphone, tablet, or computer. This is not a chatbot offering generic advice. This is a sophisticated medical AI trained on millions of patient cases, current medical literature, and your personal health history.
The AI assistant serves as your first point of contact for any health concern. It can assess symptoms through conversational interface and guided questions, analyze your descriptions of problems in the context of your complete medical history, provide immediate guidance on home care for minor issues, determine when you need to speak with a human doctor, schedule virtual or in-person appointments, remind you about medications and preventive care, track chronic conditions and alert you to concerning trends, and answer questions about medications, treatments, or health concerns anytime you have them.
The AI learns your personal health patterns over time, becoming more effective at identifying when something is wrong. It might notice that your usual minor allergy symptoms are more severe this season, or that your sleep patterns have changed in ways that correlate with depression, or that your descriptions of fatigue match patterns seen in early diabetes. This continuous, personalized monitoring provides a level of preventive care impossible in traditional medicine where you see a doctor for fifteen minutes every year.
The AI doesn't replace human doctors but rather enhances them. When you need to speak with a physician, the AI has already gathered relevant information, analyzed your symptoms, and prepared a preliminary assessment. The doctor can focus on judgment, empathy, and decision-making rather than routine information gathering.
Virtual Physicians: Human Expertise at Scale
When the AI determines you need human medical expertise, you're connected immediately to a licensed physician via video consultation. These are real doctors with full medical training, but they're augmented by AI tools that make them dramatically more effective.
During your video consultation, the physician has instant access to your complete medical history, the AI's preliminary assessment and analysis, real-time clinical decision support drawing on current medical literature, diagnostic algorithms that can analyze visible symptoms, and the ability to order labs, imaging, or prescriptions immediately.
The AI assists the physician throughout the consultation, surfacing relevant information, suggesting diagnostic possibilities the doctor might not have considered, checking for drug interactions when prescribing, and ensuring nothing important is overlooked. The doctor maintains full control and makes all decisions, but does so with the support of an intelligence that has analyzed millions of similar cases.
This combination of AI efficiency and human judgment creates something unprecedented: highly personalized, expert medical care available to everyone, instantly, at no cost. For the vast majority of medical needs (infections, rashes, minor injuries, prescription refills, mental health support, chronic disease management), this virtual care is not just adequate but superior to traditional office visits. No waiting rooms. No taking time off work. No transportation barriers. Just immediate access to expert care.
When physical examination, testing, or procedures are needed, the virtual physician coordinates everything, ordering labs or imaging at regional facilities, referring to specialists when necessary, and following up on results. The virtual doctor becomes your continuous medical partner, managing your care across all providers and maintaining the thread of your health story throughout your life.
Regional Health Centers: Physical Care When Needed
While AI-enhanced virtual care handles most medical needs, some situations require physical presence. Universal Basic Healthcare includes a comprehensive network of Regional Health Centers where Americans receive in-person services at no cost.
These modern facilities provide blood work and comprehensive lab testing, diagnostic imaging including X-rays, ultrasounds, and MRIs, vaccinations and immunizations, basic physical examinations, wound care and minor procedures, preventive screenings, health and wellness consultations, and coordination with specialists when needed.
Regional Health Centers operate on an efficient appointment system coordinated through the virtual care platform. Your AI assistant or virtual physician schedules your visit, the facility knows exactly what services you need before you arrive, results flow immediately back to your care team, and follow-up is handled through the virtual system.
By separating routine and preventive care from emergency services, we dramatically reduce the burden on hospitals and emergency rooms, allowing them to focus on genuine emergencies and complex cases. This alone saves billions while improving outcomes for both routine and critical care.
The Healthcare Account: $10,000 for Every Child
Beyond covering basic medical needs, Universal Basic Healthcare provides real financial security through Healthcare Accounts. Every child born in America receives an account seeded with $10,000, available throughout their life for healthcare expenses beyond basic services.
The Healthcare Account covers specialist consultations when referral is needed, elective procedures not covered by basic care, dental care beyond basic preventive services, vision care including corrective lenses and procedures, extended mental health services and therapy, physical therapy and rehabilitation, prescription medications outside the basic formulary, alternative and complementary medicine when desired, and any other legitimate medical expense the individual chooses.
Birth and early childhood care (prenatal care, delivery, well-baby visits, childhood vaccinations) are covered entirely by the basic system. The Healthcare Account supplements this, available for any additional needs from specialized pediatric care to unexpected medical situations.
Parents control the account for minor children, making decisions about care while having resources to pay for it. As children become adults, control transfers to them. The account provides genuine healthcare security during the critical early decades of life when many Americans have the least financial cushion but face real medical needs.
By age 50, most Americans will have used only a portion of their Healthcare Account, having been kept healthy by preventive care, good nutrition, and early intervention when issues arise. Others will have depleted it but will have had access to necessary care throughout their lives. Either way, the anxiety of "can I afford to see a doctor?" is eliminated for the majority of healthcare encounters Americans experience.
Optional Insurance for Aging and Long-Term Care
Universal Basic Healthcare covers approximately 90% of healthcare needs for most Americans from birth through middle age. But as Americans age beyond 50, healthcare needs typically increase. For this stage of life, Americans can purchase optional insurance from a competitive national marketplace.
This insurance is truly optional. It's not required by law, not tied to employment, and not necessary for basic care, which remains free and accessible throughout life. Instead, it functions like life insurance—a personal choice to protect against the significant healthcare costs that often come with aging.
The National Healthcare Marketplace
The marketplace operates as a genuinely competitive national system where insurance companies offer products designed specifically for the 50-80+ age group. These policies focus on the healthcare needs of older Americans: coverage for chronic disease management beyond basic care, major surgical procedures, cancer treatment and advanced therapies, long-term care including nursing home and in-home care, advanced imaging and diagnostic procedures, specialist networks for complex conditions, prescription drug coverage for expensive medications, and comprehensive end-of-life care.
Because this insurance is optional and supplementary rather than the only access to care, companies compete on actual value rather than on being the only option. Prices reflect real risk rather than the distorted economics of our current system. Coverage is portable: your insurance isn't tied to your job and moves with you anywhere in the country.
Americans can purchase this insurance at any point. Some might buy it at 45 to lock in lower rates before age-related price increases. Others might wait until 60 when they anticipate needing more significant care. Some might never purchase it, relying on their Healthcare Account and basic services throughout their lives. The choice is theirs to make based on their circumstances, family history, and risk tolerance.
Long-Term Care Coverage
A crucial component of marketplace insurance is long-term care coverage, which addresses one of the most significant financial risks Americans face in later life. Traditional long-term care insurance is expensive and often inadequate. In the Universal Basic Healthcare marketplace, long-term care options are integrated into comprehensive aging care policies.
These policies can cover in-home care services allowing people to age in place, assisted living facilities for those who need support but not intensive medical care, nursing home care for those requiring continuous medical supervision, hospice and palliative care, respite care for family caregivers, and home modifications and medical equipment.
Because these policies are offered in a competitive national marketplace and supplementing rather than replacing basic care, they can be more comprehensive and affordable than traditional long-term care insurance. Insurers compete on coverage quality, service networks, and price, driving innovation in how we care for aging Americans.
How This Transforms American Healthcare
The implications of Universal Basic Healthcare extend far beyond simply providing access to doctors. This system fundamentally restructures how healthcare operates in America and, more importantly, how Americans relate to their health.
Prevention Becomes the Default
When healthy food is subsidized and junk food is not, when children learn nutrition and wellness from elementary school onward, when everyone has immediate access to medical care through AI assistants, the entire orientation of healthcare shifts from treatment to prevention.
Minor health issues are addressed before they become major ones. Chronic conditions are caught early when they're most manageable. Lifestyle interventions happen at the point where they're most effective. The result is a healthier population that needs less intensive medical care even as they age.
Healthcare Costs Decline While Health Improves
This seems paradoxical but it's inevitable. Early intervention prevents expensive late-stage treatment. Good nutrition reduces the incidence of metabolic diseases that currently consume huge percentages of healthcare spending. AI-enhanced virtual care delivers expert diagnosis and treatment at a fraction of the cost of traditional office visits. Healthy aging means more productive years and less intensive care in later life.
America currently spends over $4 trillion annually on healthcare, much of it treating preventable chronic diseases. Universal Basic Healthcare redirects resources toward prevention, early intervention, and efficient delivery, achieving better outcomes at lower total cost.
Health Equity Becomes Reality
Under the current system, your health outcomes correlate strongly with your zip code, income, and insurance status. Under Universal Basic Healthcare, every American has access to the same AI health assistant, the same virtual physicians, the same regional health centers, and the same financial resources through Healthcare Accounts.
The child born into poverty has access to the same preventive care, the same nutritious food subsidies, and the same $10,000 Healthcare Account as the child born into wealth. Health outcomes will always vary based on genetics and circumstances, but access to care and resources becomes truly equal.
Innovation Flourishes in New Directions
With basic care universally provided, healthcare innovation focuses on genuine improvements rather than on gaming insurance reimbursements or exploiting information asymmetries. Companies compete to build better AI diagnostic tools, more effective virtual care platforms, superior regional health facilities, and innovative insurance products for older Americans.
Medical AI development accelerates as millions of patient interactions generate data that improves diagnostic accuracy. Virtual care platforms evolve to handle increasingly complex cases. The insurance marketplace drives innovation in long-term care delivery and aging services. Competition rewards those who improve outcomes and efficiency, not those who maximize billing.
The Doctor-Patient Relationship Evolves
Physicians freed from administrative burdens and empowered by AI can focus on what they do best: applying medical judgment, providing empathy and support, making complex decisions, and building relationships with patients. The AI handles routine information gathering, preliminary analysis, and documentation. The doctor focuses on the human elements of medicine that AI cannot replace.
Virtual care allows doctors to maintain continuous relationships with patients rather than seeing them for fifteen minutes once a year. The combination of AI monitoring and regular virtual check-ins means doctors know their patients better and can intervene earlier when issues arise.
Addressing Concerns and Challenges
Any major restructuring of a system as large and complex as American healthcare faces legitimate questions and concerns.
Won't this be incredibly expensive? Less expensive than the current system. Virtual care costs a fraction of traditional office visits. AI assistance allows physicians to serve more patients more effectively. Preventing disease through nutrition and education is vastly cheaper than treating chronic conditions. The $10,000 Healthcare Account is a one-time investment that replaces ongoing subsidies and emergency care costs. Most importantly, a healthier population requires less intensive care throughout life.
Can AI really provide quality medical care? AI doesn't provide care; doctors do. AI enhances human medical expertise, handling information analysis, pattern recognition, and routine assessment while physicians provide judgment, empathy, and decision-making. Current medical AI already matches or exceeds human performance on many diagnostic tasks. Combined with human expertise, the quality of care exceeds what either could provide alone.
What if I prefer traditional in-person doctors? You can see them. Healthcare Accounts and optional insurance can be used for traditional office visits if you prefer that experience. Universal Basic Healthcare doesn't eliminate traditional medicine; it supplements it with more efficient options while ensuring everyone has access to basic care. Doctors who provide superior in-person care will thrive.
Won't food companies fight the MAHA standards? Some will, others will adapt. Food industry consolidation has created companies that sell both healthy and unhealthy products. They'll shift production toward products that meet standards. Smaller innovative companies will emerge to provide healthy alternatives. The transition has already begun with companies reformulating products and introducing healthier options. MAHA standards accelerate an inevitable shift.
How do we prevent abuse of free basic care? Professional medical judgment. AI systems can identify unusual usage patterns. Physicians manage care appropriately. But mostly, we accept that some level of utilization is not "abuse" but people finally having access to care they previously couldn't afford. If utilization increases, that likely means we're catching and treating problems earlier, which saves money in the long run.
What about people who don't want to buy insurance in later life? That's their choice. Basic care remains free and accessible throughout life. Healthcare Accounts continue to be available. Optional insurance is for those who want additional coverage for major medical events and long-term care. Some people will rationally choose to self-insure or accept the risks. That's freedom.
Isn't this just socialism? It's pragmatic use of technology to ensure basic access while preserving choice and competition. Virtual care is cheaper than traditional care: why not make it universally available? Good nutrition education helps people stay healthy; why not provide it? Healthcare Accounts and optional insurance preserve individual choice and market competition. This is technology-enabled abundance, not government control.
Implementation and Timeline
Universal Basic Healthcare can be implemented systematically over a six-year period, with immediate benefits emerging at each phase.
Year One: Foundation and Education begins with implementing MAHA nutritional standards and food subsidy programs, launching comprehensive wellness education in schools starting with elementary grades, developing AI health assistant platforms and beginning training on medical data, recruiting and training physicians for virtual care system, and establishing regulatory framework for national insurance marketplace.
Year Two: AI and Virtual Launch deploys AI health assistants in pilot regions with millions of users, launches virtual physician network with AI support in pilot areas, begins construction and retrofitting of Regional Health Centers, establishes Healthcare Accounts for all newborns, and collects data on system performance and medical outcomes from pilot programs.
Year Three: National Rollout Begins with AI health assistants available to all Americans nationwide, virtual physician care accessible in all regions, first Regional Health Centers opening in major metropolitan areas, Healthcare Accounts opened for all children under age 18, and continued expansion of food subsidies and nutritional standards.
Year Four: System Maturation completes Regional Health Center network across the nation, refines AI diagnostic capabilities based on data from millions of patient interactions, expands virtual care capabilities to handle increasingly complex cases, launches optional insurance marketplace for 50+ age group, and analyzes health outcomes data showing early results from prevention focus.
Year Five: Integration and Optimization achieves full integration between AI assistants, virtual physicians, Regional Health Centers, and specialist networks. The system demonstrates measurable improvements in health outcomes and cost efficiency, insurance marketplace competition drives innovation in aging care coverage, Healthcare Accounts show substantial balances for most young adults, and nutritional interventions show measurable impacts on chronic disease rates.
Year Six: Full Operation sees Universal Basic Healthcare operating at full scale with all components mature. Health outcomes data demonstrates system effectiveness, cost savings become apparent in both government spending and household budgets, optional insurance marketplace offers diverse competitive products for older Americans, and the system establishes itself as the new standard of American healthcare.
A Healthier, More Prosperous America
Universal Basic Healthcare is ultimately about recognizing that health is the foundation of human flourishing. When people are healthy, they're more productive, more creative, more engaged in their communities, and better able to pursue their aspirations. When children grow up learning about nutrition and wellness, they make better choices throughout life. When everyone can access medical care without financial anxiety, they address problems early rather than letting them fester into crises.
This system preserves what works in American healthcare (innovation, choice, competition) while fixing what doesn't: access, affordability, prevention, and the basic security of knowing you can see a doctor when you need one. It's not socialized medicine and it's not the status quo. It's a technology-enabled approach that provides universal access to essential services while maintaining the dynamism and innovation that competition delivers.
The transformation extends beyond healthcare itself. When Americans are healthier, they miss less work, learn better in school, start more businesses, and contribute more to their communities. When families aren't bankrupted by medical bills, they invest in education, housing, and their children's futures. When young adults have healthcare security, they take entrepreneurial risks that drive economic growth. When older Americans have affordable options for long-term care, they age with dignity rather than fear.
The question is not whether we can afford Universal Basic Healthcare. We already spend more per capita on healthcare than any nation on Earth while getting worse outcomes. The question is whether we have the will to restructure a system that enriches a few while failing millions, replacing it with one that uses modern technology and preventive approaches to deliver genuine health for all.
In a nation of abundance, healthcare abundance should be within reach. Universal Basic Healthcare makes it reality, building a foundation of health upon which Americans can construct lives of achievement, purpose, and fulfillment. The future of American healthcare is not more of the same. It's something fundamentally better, and it's within our grasp.
